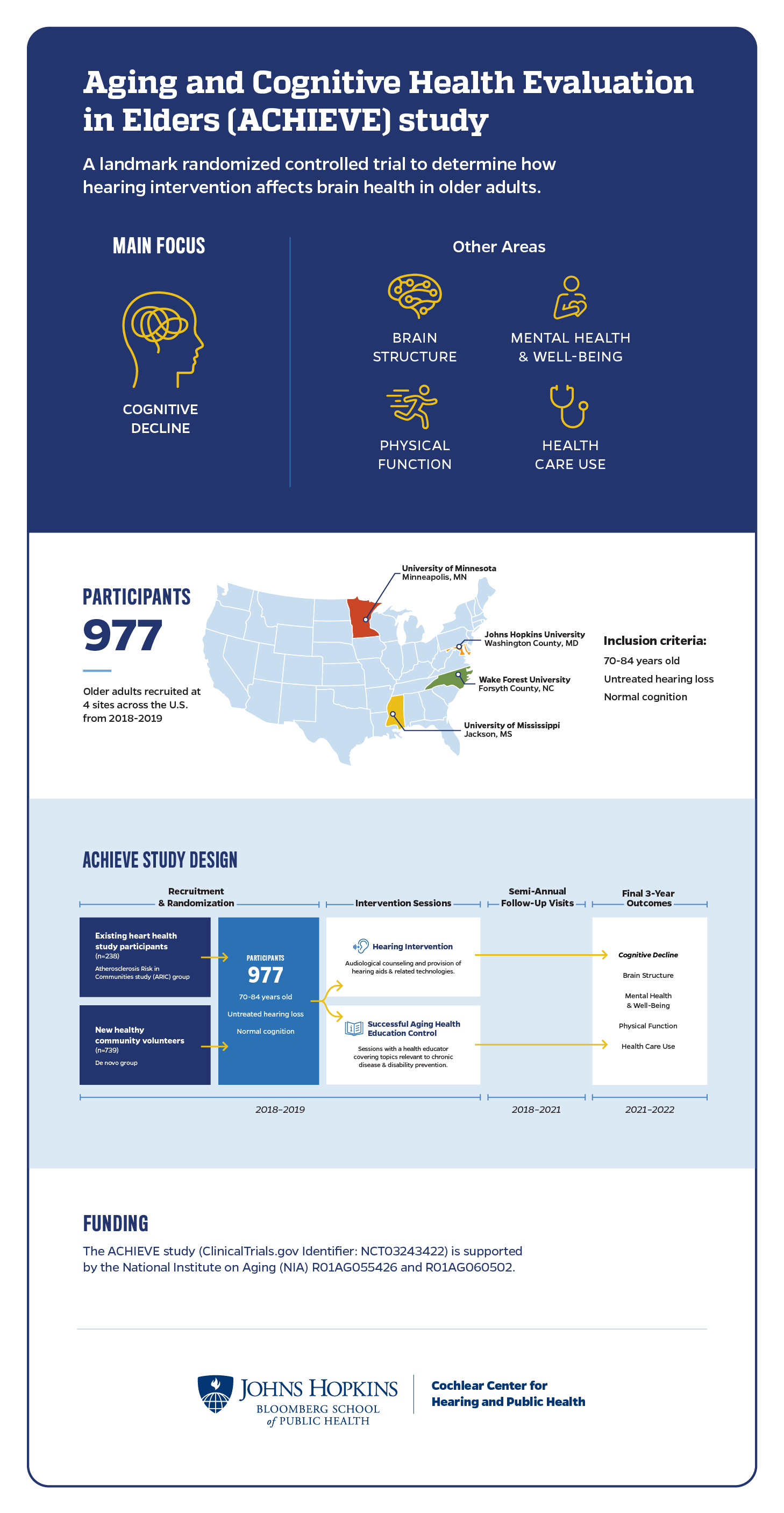
The Aging and Cognitive Health Evaluation in Elders, or ACHIEVE, study is a multicenter, randomized controlled trial designed to determine if treating hearing loss in older adults reduces cognitive decline over a three-year period.
The ACHIEVE study also looks at the effects of treating hearing loss on other health outcomes, including mental health and well-being, physical function, and health care use.
The ACHIEVE study involved 977 older adults ages 70-84 years with untreated hearing loss. Participants in the ACHIEVE study came from two distinct study populations: a group of adults who were already participating in a heart health study and a group of healthy volunteers who were newly recruited from the community. The 238 participants who came from the heart health study were, on average, older and had more risk factors for cognitive decline than the 739 new healthy community volunteers.
Study participants were randomly assigned to either a hearing intervention or a health education control intervention. Study participants were then followed for three years with semi-annual visits where researchers collected data about their thinking and memory abilities, and mental and physical health.